Fibromyalgia Syndrome (FMS)
Fibromyalgia Syndrome
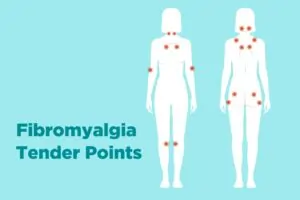
Fibromyalgia is a disease of abnormal pain perception and is one of the most common causes of chronic widespread pain.
It is characterised by reduced pain thresholds and heightened sensitivity to normally harmless stimuli. Fibromyalgia affects about 2% of the general population, with females being seven times more susceptible than men.While it is an independent syndrome, it often coexists with other conditions such as rheumatoid arthritis, systemic lupus erythematosus, and chronic pain disorders like low back pain and headaches.
Clinical Features of Fibromyalgia:
Widespread Pain: Patients often describe “pain all over their body,” with severity varying among individuals. Exertion or physical activity may worsen the pain.
Fatigue: 80–90% of fibromyalgia patients experience extreme tiredness, ranging from mild to severe exhaustion.
Poor Sleep Quality: Many patients struggle with poor-quality sleep and do not feel refreshed even after a full night’s rest.
Depression and Anxiety: Mood disturbances are common, with generalized anxiety being more prevalent than depression.
Impaired Cognition: Patients often experience “brain fog,” leading to memory issues, difficulty focusing, and trouble with problem-solving.
Morning Stiffness: Unlike other inflammatory conditions, stiffness in fibromyalgia is not relieved by exercise.
Other Symptoms: Common symptoms include nausea, bloating, abdominal pain, diarrhea, constipation, and symptoms of irritable bowel syndrome. Uro-gynecological symptoms like urgency, frequency, incontinence, pelvic pain, and dysmenorrhea are also frequent.
Diagnosis of Fibromyalgia:
Diagnosis is based on clinical signs and symptoms. There are no specific laboratory tests for fibromyalgia, but blood tests help rule out other rheumatic diseases.
Risk Factors:
Psychological conditions such as depression, anxiety, and mood disorders increase the risk of developing fibromyalgia. Genetic predisposition, infections, hormonal changes, physical trauma (e.g., car accidents), and stress are also linked to the syndrome.
Fibromyalgia Treatment in Pune:
Treatment focuses on improving symptoms and enhancing quality of life. Since fibromyalgia presents with various symptoms, treatment is individualized to address the most distressing aspects. Both pharmacological and non-pharmacological approaches are utilized.
Non-Pharmacological Treatment:
Patient Education: Since fibromyalgia is a chronic condition with no permanent cure, educating patients on managing their pain is crucial.
Graded Exercises: Initially, exercise may worsen pain and fatigue, but gradual increase helps improve physical function.
Physical Therapy: A physical therapist can teach exercises to enhance strength, flexibility, and stamina. Water-based exercises are particularly beneficial.
Counseling: Talking to a counselor helps develop coping strategies for stress management.
Pharmacological Treatments:
Analgesics: NSAIDs may provide short-term pain relief but should be used cautiously due to gastrointestinal side effects.
Tricyclic Antidepressants (TCA): Amitriptyline is commonly used to improve sleep, fatigue, and pain.
SNRIs (Serotonin-Norepinephrine Reuptake Inhibitors): Medications such as milnacipran, duloxetine, and venlafaxine help alleviate pain, fatigue, and cognitive issues.
SSRIs (Selective Serotonin Reuptake Inhibitors): Fluoxetine and paroxetine may also be beneficial.
Anticonvulsants: Pregabalin and gabapentin, originally used for epilepsy, are effective in managing fibromyalgia-related pain.
For expert care and personalized Fibromyalgia Treatment in Pune, consulting a specialist can help patients manage their condition effectively and improve their quality of life.